Oedema is swelling caused by excess fluid trapped in your body’s tissues. Although oedema can affect any part of your body, you may notice it more in your hands, arms, feet, ankles and legs.
Oedema can be the result of medication, pregnancy or an underlying disease — often congestive heart failure, kidney disease or cirrhosis of the liver.
Taking medication to remove excess fluid and reducing the amount of salt in your food often relieves oedema. When edema is a sign of an underlying disease, the disease itself requires separate treatment.
Symptoms
Signs of Oedema include:
- Swelling or puffiness of the tissue directly under your skin, especially in your legs or arms
- Stretched or shiny skin
- Skin that retains a dimple (pits), after being pressed for several seconds
- Increased abdominal size
Causes
Oedema occurs when tiny blood vessels in your body (capillaries) leak fluid. The fluid builds up in surrounding tissues, leading to swelling.
Mild cases of Oedema may result from:
- Sitting or staying in one position for too long
- Eating too much salty food
- Having premenstrual signs and symptoms
- Being pregnant
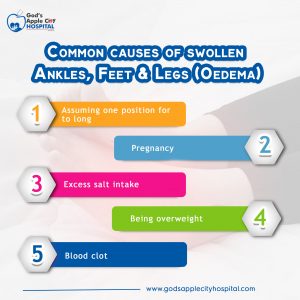
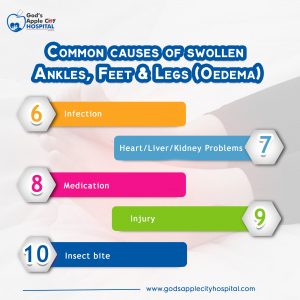
Oedema can also be a side effect of some medications, including:
- High blood pressure medications
- Nonsteroidal anti-inflammatory drugs
- Steroid drugs
- Estrogens
- Certain diabetes medications called thiazolidinediones
In some cases, however, Oedema may be a sign of a more serious underlying medical condition. Several diseases and conditions may cause oedema, including:
- Congestive heart failure. If you have congestive heart failure, one or both of your heart’s lower chambers lose their ability to pump blood effectively. As a result, blood can back up in your legs, ankles and feet, causing oedema. Congestive heart failure can also cause swelling in your abdomen. Sometimes, this condition can cause fluid to accumulate in your lungs (pulmonary oedema), which can lead to shortness of breath.
- Cirrhosis. Fluid may accumulate in your abdominal cavity (ascites) and in your legs as a result of liver damage (cirrhosis).
- Kidney disease. When you have kidney disease, extra fluid and sodium in your circulation may cause oedema. The oedema associated with kidney disease usually occurs in your legs and around your eyes.
- Kidney damage. Damage to the tiny, filtering blood vessels in your kidneys can result in nephrotic syndrome. In nephrotic syndrome, declining levels of protein (albumin) in your blood can lead to fluid accumulation and oedema.
- Weakness or damage to veins in your legs. If you have chronic venous insufficiency, the one-way valves in your leg veins are weakened or damaged, which allows blood to pool in your leg veins and causes swelling. Sudden onset of swelling in one leg accompanied by pain in your calf muscle can be due to a blood clot (deep vein thrombosis, or DVT) in one of your leg veins. If this occurs, seek medical help immediately.
- Inadequate lymphatic system. Your body’s lymphatic system helps clear excess fluid from tissues. If this system is damaged for example, by cancer surgery the lymph nodes and lymph vessels draining an area may not work correctly, and oedema can occur.
- Severe, long-term protein deficiency. An extreme lack (deficiency), of protein in your diet over a long period of time can lead to fluid accumulation and oedema.
Risk factors
If you are pregnant, your body retains more sodium and water than usual due to the fluid needed by the fetus and placenta. This can increase your risk of developing oedema.
A chronic illness such as congestive heart failure or liver or kidney disease can increase your risk of oedema. Also, surgery can sometimes obstruct a lymph node, leading to swelling in an arm or leg, usually on just one side.
Complications
If left untreated, oedema can cause:
- Increasingly painful swelling
- Difficulty walking
- Stiffness
- Stretched skin, which can become itchy and uncomfortable
- Increased risk of infection in the swollen area
- Scarring between layers of tissue
- Decreased blood circulation
- Decreased elasticity of arteries, veins, joints and muscles
- Increased risk of skin ulcers
Diagnosis
To understand what might be causing your oedema, your doctor will first perform a physical exam and ask you questions about your medical history. This information is often enough to determine the underlying cause of your oedema. In some cases, X-rays, ultrasound exams, magnetic resonance imaging, blood tests or urine analysis may be necessary.
Treatment
Mild oedema usually goes away on its own, particularly if you help things along by raising the affected limb higher than your heart.
More-severe oedema may be treated with drugs that help your body expel excess fluid in the form of urine (diuretics). One of the most common diuretics is furosemide (Lasix). However, your doctor will determine whether these types of medications are a good option for you based on your personal medical history.
Long-term management typically focuses on treating the underlying cause of the swelling. If oedema occurs as a result of medication use, your doctor may adjust your prescription or check for an alternative medication that doesn’t cause oedema.
Lifestyle and home remedies
The following may help decrease oedema and keep it from coming back. Before trying these self-care techniques, talk to your doctor about which ones are right for you.
- Movement. Moving and using the muscles in the part of your body affected by oedema, especially your legs, may help pump the excess fluid back toward your heart. Ask your doctor about exercises you can do that may reduce swelling.
- Elevation. Hold the swollen part of your body above the level of your heart several times a day. In some cases, elevating the affected body part while you sleep may be helpful.
- Massage. Stroking the affected area toward your heart using firm, but not painful, pressure may help move the excess fluid out of that area.
- Compression. If one of your limbs is affected by oedema, your doctor may recommend you wear compression stockings, sleeves or gloves, usually worn after your swelling has gone down, to prevent further swelling from occurring. These garments keep pressure on your limbs to prevent fluid from collecting in the tissue.
- Protection. Keep the affected area clean, moisturized and free from injury. Dry, cracked skin is more prone to scrapes, cuts and infection. Always wear protection on your feet if that’s where the swelling typically occurs.
- Reduce salt intake. Follow your doctor’s suggestions about limiting how much salt you consume. Salt can increase fluid retention and worsen oedema.
When to see a doctor
Make an appointment to see your doctor if you have swelling, stretched or shiny skin, or skin that retains a dimple after being pressed (pitting). See your doctor immediately if you experience:
- Shortness of breath
- Difficulty breathing
- Chest pain
These can be signs of pulmonary oedema, which requires prompt treatment.
If you’ve been sitting for a prolonged period, such as on a long flight, and you develop leg pain and swelling that won’t go away, call your doctor. Persistent leg pain and swelling can indicate a blood clot deep in your vein (deep vein thrombosis, or DVT).
.
.
.
.
.
.
.
.
.
.
.
.
.
.
Kindly Check us out on
Facebook @ godsapple.hospital
Instagram @ godsapplecityhospital
Click on the link below to read other posts:
