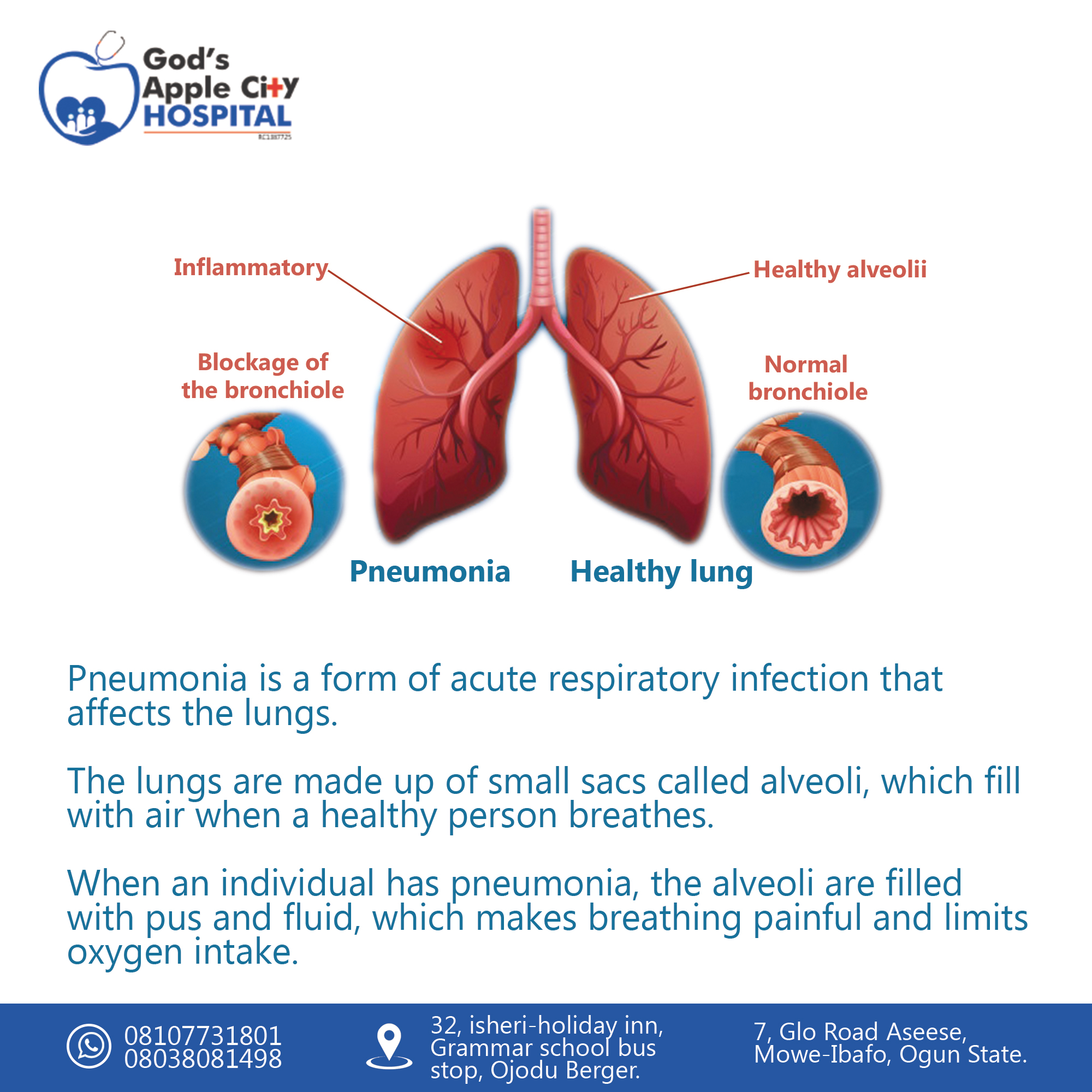
Pneumonia
Pneumonia is a form of acute respiratory infection that affects the lungs. The lungs are made up of small sacs called alveoli, which fill with air when a healthy person breathes. When an individual has pneumonia, the alveoli are filled with pus and fluid, which makes breathing painful and limits oxygen intake.
Causes
Pneumonia happens when germs get into your lungs and cause an infection. The immune system’s reaction to clear the infection results in inflammation of the lung’s air sacs (alveoli). This inflammation can eventually cause the air sacs to fill up with pus and liquids, causing pneumonia symptoms.
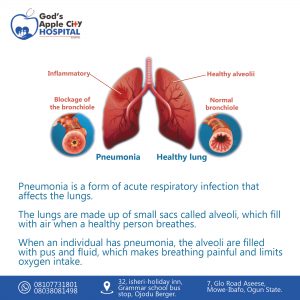
Several types of infectious agents can cause pneumonia, including bacteria, viruses, and fungi.
Bacterial pneumonia
The most common cause of bacterial pneumonia is Streptococcus pneumoniae. Other causes include:
- Mycoplasma pneumoniae
- Haemophilus influenzae
- Legionella pneumophila
Viral pneumonia
Respiratory viruses are often the cause of pneumonia. Examples of viral infections that can cause pneumonia include:
- influenza (flu)
- respiratory syncytial virus (RSV)
- rhinoviruses (common cold)
- human parainfluenza virus (HPIV) infection
- human metapneumovirus (HMPV) infection
- measles
- chickenpox (varicella-zoster virus)
- adenovirus infection
- coronavirus infection
SARS-CoV-2 infection (the virus that causes COVID-19)
Although the symptoms of viral and bacterial pneumonia are very similar, viral pneumonia is usually milder. It can improve in 1 to 3 weeks without treatment.
According to the National Heart, Lung, and Blood Institute, people with viral pneumonia are at risk of developing bacterial pneumonia.
Fungal pneumonia
Fungi from soil or bird droppings can cause pneumonia. They most often cause pneumonia in people with weakened immune systems. Examples of fungi that can cause pneumonia include:
- Pneumocystis jirovecii
- Cryptococcus species
- Histoplasmosis species
Symptoms of Pneumonia
- Fever
- Chest pain
- Sputum cough
- Headache
- Pallor of the skin
- Sweating
- Muscle aches
- Fatigue
- Shortness of breath
- Nausea

Risk factors
Anyone can get pneumonia, but certain groups do have a higher risk. These groups include:
- Infants from birth to 2 years old
- People ages 65 and older
- People with weakened immune systems due to: Pregnancy, HIV
Diagnosis
Your doctor will start by taking your medical history. They’ll ask you questions about when your symptoms first appeared and your health in general.
They’ll then give you a physical exam. This will include listening to your lungs with a stethoscope for any abnormal sounds, such as crackling.
Depending on the severity of your symptoms and your risk of complications, your doctor may also order one or more of these tests:
Chest X-ray
An X-ray helps your doctor look for signs of inflammation in your chest. If inflammation is present, the X-ray can also inform your doctor about its location and extent.
Blood culture
This test uses a blood sample to confirm an infection. Culturing can also help identify what may be causing your condition.
Sputum culture
During a sputum culture, a sample of mucus is collected after you’ve coughed deeply. It’s then sent to a lab to be analyzed to identify the cause of the infection.
Pulse oximetry
A pulse oximetry measures the amount of oxygen in your blood. A sensor placed on one of your fingers can indicate whether your lungs are moving enough oxygen through your bloodstream.
CT scan
CT scans provide a clearer and more detailed picture of your lungs.
Fluid sample
If your doctor suspect there’s fluid in the pleural space of your chest, they may take a fluid sample using a needle placed between your ribs. This test can help identify the cause of your infection.
Bronchoscopy
A bronchoscopy looks into the airways in your lungs. It does this using a camera on the end of a flexible tube that’s gently guided down your throat and into your lungs.
Your doctor may do this test if your initial symptoms are severe, or if you’re hospitalized and not responding well to antibiotics.
Treatment
Your treatment will depend on the type of pneumonia you have, how severe it is, and your general health.
Prescription medications
Your doctor may prescribe a medication to help treat your pneumonia. What you’re prescribed will depend on the specific cause of your pneumonia.
Oral antibiotics can treat most cases of bacterial pneumonia. Always take your entire course of antibiotics, even if you begin to feel better. Not doing so can prevent the infection from clearing, and it may be harder to treat in the future.
Antibiotic medications don’t work on viruses. In some cases, your doctor may prescribe an antiviral. However, many cases of viral pneumonia clear on their own with at-home care.
Antifungal medications are used to treat fungal pneumonia. You may have to take this medication for several weeks to clear the infection.
OTC medications
Your doctor may also recommend over-the-counter (OTC) medications to relieve your pain and fever, as needed. These may include:
- Aspirin
- Ibuprofen (Advil, Motrin)
- Acetaminophen (Tylenol)
Your doctor may also recommend cough medicine to calm your cough so you can rest. Keep in mind coughing helps remove fluid from your lungs, so you don’t want to eliminate it entirely.
Home remedies
Although home remedies don’t actually treat pneumonia, there are some things you can do to help ease symptoms.
Coughing is one of the most common symptoms of pneumonia. Natural ways to relieve a cough include gargling salt water or drinking peppermint tea.
Cool compresses can work to relieve a fever. Drinking warm water or having a nice warm bowl of soup can help with chills. Here are more home remedies to try.
You can help your recovery and prevent a recurrence by getting a lot of rest and drinking plenty of fluids.
Although home remedies can help ease symptoms, it’s important to stick to your treatment plan. Take any prescribed medications as directed.
Hospitalization
If your symptoms are very severe or you have other health problems, you may need to be hospitalized. At the hospital, doctors can keep track of your heart rate, temperature, and breathing. Hospital treatment may include:
- Antibiotics injected into a vein
- Respiratory therapy, which involves delivering specific medications directly into the lungs, or teaching you to perform breathing exercises to maximize your oxygenation
- Oxygen therapy to maintain oxygen levels in your bloodstream (received through a nasal tube, face mask, or ventilator, depending on severity)
.
.
.
.
.
.
.
.
https://web.facebook.com/Godsapplecity
read other blogs https://godsapplecityhospital.com/breast-cancer-signs-and-detection/